Acute Coronary Syndromes
Checklist
- ECG: Get a 12 lead ECG within 10 minutes of patient presenting with chest pain
- Vitals: Take initial vital signs: temp, HR, RR, SpO2, BP in both arms; and repeat if there further chest pain or equivalent symptoms
- Oxygen: Give Oxygen if SpO2 ≤ 90% or there are clinical signs of hypoxemia
- Antiplatelets: Give acetylsalicylic acid (Aspirin®) now if it was not given prior to arrival at hospital. Write down when it was given.
- Nitroglycerin: Give Nitroglycerin in hemodynamically stable patients every 5 minutes as needed. *Avoid if suspected RV infarction. Dose: usually 0.3 to 0.4 mg.
- Place defibrillation pads on chest – because there is a high risk of VF/ pulseless VT.
- Monitor ECG and include rhythm strip – looking out for arrhythmias.
- Determine eligibility for reperfusion
- Determine eligibility for fibrinolysis aka thrombolysis
- Do they have any absolute contraindications? Do not memorize the list, there will be a check list.
Approach to the patient with chest pain
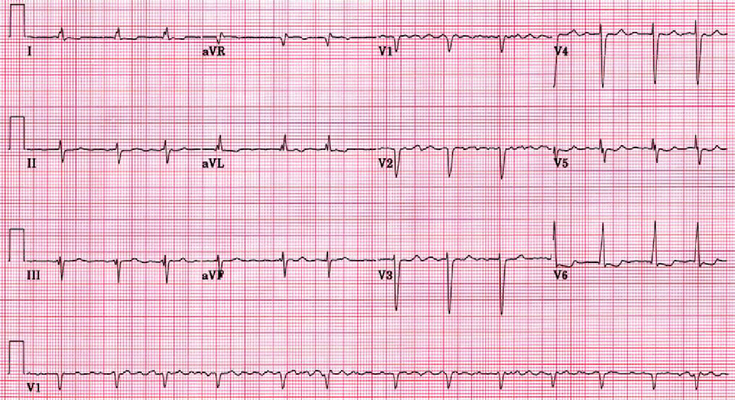
The first step is to get a 12 lead ECG, looking for ST elevation or other ECG changes indicating myocardial infarction. The ECG should be done as quickly as possible after arrival at hospital with chest pain, the goal is within 10 minutes! If there is ST elevation, then likely a STEMI, and they need to go to the catheter lab right away (emergent).
STEMI diagnosis only the positive ECG! No labs (i.e. troponins needed).
STEMI criteria = ST segment elevation of ≥1 mm in 2 contiguous leads with or withouts signs and symptoms of ACS. Continguous leads refers to lead groups such as anterior leads (V1-V6), inferior leads (II, III, aVF), or lateral/apical leads (I, aVL). Supplemental leads such as V3R/V4R reflect the free wall of the right ventricle and V7-V9 the infero-basal wall.
If the 12 lead ECG is normal, then the next step is to get troponin I, and if positive, they need to go to the catheter lab urgently.
If the troponin I is normal, then get a stress test, and if it is positive, they still need to go to the catheter lab, but now it is an elective procedure.
If the stress test is normal, this rules out coronary artery disease with ≥70% stenosis.
Note: All patients with chest pain are admitted to the hospital, and as they go through the above tests, they also need to be managed medically.
Medical Management
Stabilize Patient
First response is always the ABCs. If the patient is hypotensive, SBP < 110 mmHg, then give 250 ml NS bolus, max is 1L NS and monitor breath sounds.
Establish IV access at TKO rate or saline block.
MONA-BASH-C
Morphine, Oxygen, Nitroglycerin, Aspirin, Beta blockers, ACEI/ARBs, Statin, Heparin, Clopidogrel. The controversy is over the first three.
Patients need pain relief and nitroglycerin is the first choice for this, however, if it is not enough two common options are morphine and fentanyl.
Nitroglycerin
Sublingual nitroglycerin as 0.4 mg tablet or as a spray is given every 5 minutes until pain is gone or until 3 doses have been given (maximum amount). This is done before arriving at the hospital by paramedics.
DO not give nitroglycerin to patients who use Sildenafil (Viagra®) or Vardenafil (Levitra®) in the last 24 hours or who have used Tadalafil (Cialis®) within the last 36 hours. Combination of nitroglycerin with these phosphodiesterase inhibitors (PDE5), can cause severe hypotension.
Nitroglycerin works by both dilating coronary blood vessels and by decreasing the workload of the heart. It directly relaxes vascular smooth muscle. At low doses it mainly dilates veins, and venodilation promotes pooling of blood in the peripheral vessels which reduces blood return to the heart thus reducing the preload aka left ventricular diastolic pressure. This means the left ventricle has less blood to pump out or less “work”. This results in reduced myocardial oxygen demand.
For vasospastic angina (Variant, Prinzmetal) – it relaxes smooth muscle in the epicardial coronary arteries and reduces coronary artery spasm.
Aspirin
Chewable not swallowed, oral aspirin is given at the first sign of chest pain.
Dose? Alberta health services – dose is 160 mg chewed or swallowed. AHA says 324 mg chewed only.
Morphine & Fentanyl
Used as a last resort, when pain is not relieved by nitroglycerine, and in very specific scenarios. For example, they have had all the other medical therapy above, they are still in pain, and they are not in the catheter lab to be revascularized. Because it is often given to these patients, it may appear to some that morphine is associated with worse outcomes, but it is not. Do not with-hold morphine, even in addicts! If they are in pain, they need it.
Morphine dose is usually 2-4 mg slow IVP with max dose of 20 mg. Fentanyl is an alternative and is given as 1 mcg/kg every 15 minutes with a maximum dose of 200 mcg.
Abciximab
This is another antiplatelet agent, specifically a GPIIb/IIIa receptor blocker, and it is the most effective antiplatelet drug available. It is only available as an IV solution. By blocking glycoprotein IIb/IIIa receptors it prevents fibrinogen and Von Willebrand factors from binding on activated platelets. It an additional agent to consider giving to patients who have PCI planned or who have had a PCI procedure done.
What is the “Cath” lab?
The catheter lab is where a diagnostic angiogram is done, which is basically a left heart catheter. A wire is inserted into the radial or sometimes the femoral artery and is guided to the ostia of the coronary arteries, but not into the coronary arteries them selves. Then a dye is injected and imaging is used to assess for any filling defects. The defects are graded based on the number of arteries affected, the size of the defects, and the location of the arteries e.g. proximal or distal.
When a few arteries are affected, typically 1 or 2, and when they are medium in size then the patient is a good candidate for PCI or percutaneous coronary intervention.
When there are multiple arteries, i.e. ≥ 3 arteries affected and they are large, then CABG or coronary artery bypass grafting is the procedure often done.
When the affected arteries are distal, or small, then medical management is often done because it is hard to treat them with PCI or CABG.
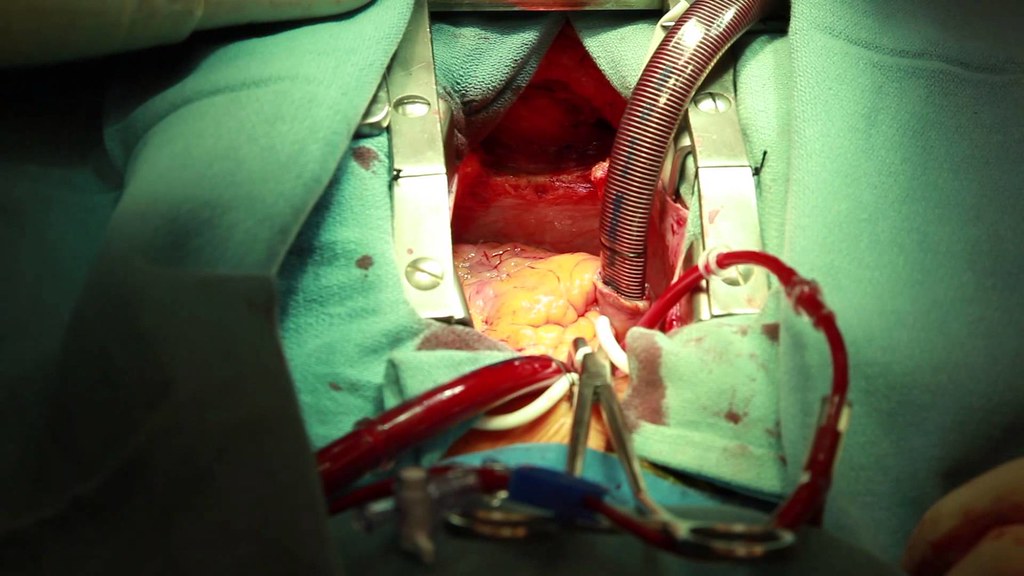
What is CABG?
Coronary artery bypass grafting. The chest and sternum are cracked open and the LIMA or left internal mammary artery is dissected and then connected to the left coronary artery to bypass the obstructed portion of the LCA.
When other arteries are affected, pieces from the great saphenous vein are used to bypass the blocks. This saphenous vein is harvested and the bypass is done across the lesion, sometimes coronary to coronary and other times aorta to coronary. The vein will undergo arterialization once it experiences the higher pressure from the arteries. The collagen will be replaced by elastin and there will be more vascular smooth muscle cells.
What is thrombolysis aka fibrinolysis?
This essentially tissue plasminogen activator or tPA. Common tPA drugs include alteplase, tenecteplase (TNK), and streptokinase. Thrombolysis is not done as often because most places have access to PCI in the USA. However, if PCI is not available or cannot be done within 90 minutes (see below for explanation as to why), then consider thrombolysis.
What is the “door to balloon time of 90 min?”
This is a requirement that is needed for accreditation as a hospital that can deal with myocardial infarctions. It means 90 minutes from the time the patient enters the hospital to the time they get angioplasty, and this includes diagnostic tests, etc. It is important for hospital management.
However, if it will take more than 60 minutes to get to a PCI capable center, then consider tPA.
Contraindications to thrombolysis
Thrombolytics will break up clots all over the body, not just at the obstructed coronary artery. So, if there was recent surgery, or trauma then those clots will also break up leading to a risk of major bleeding.
Don’t memorize the contraindications to thrombolysis, there are many checklists for this, and each institution/ hospital has its own checklist or protocol for this.
Absolute Contraindications to thrombolysis aka fibrinolysis:
- Prior intracranial hemorrhage or stroke of unknown origin at any time.
- Central nervous system damage or neoplasms, or arteriovenous malformation.
- Ischemic stroke within 6 months.
- Suspected aortic dissection.
- Active bleeding or bleeding diathesis (excluding menses).
- Significant closed head or facial trauma within 3 months.
- Major surgery within the last 3 weeks.
- Internal bleeding within the past 30 days.
- Non-compressible vascular punctures
Relative Contraindications to thrombolysis aka fibrinolysis:
- History of chronic, severe, poorly controlled hypertension.
- Severe, uncontrolled hypertension on presentation (SBP greater than 180 mmHg or DBP greater than 110 mmHg).
- Transient ischemic attack within 6 months.
- Traumatic or prolonged CPR (greater than 10 minutes).
- Pregnancy or within one week postpartum.
- Active peptic ulcer disease.
- Oral anticoagulant therapy.
- Advanced liver disease.
- Infective endocarditis.

What is PCI?
Percutaneous coronary intervention. The wire is inserted at the radial or femoral artery then advanced into the coronary artery, unlike diagnostic angiogram where it stops at the ostia of the coronary artery. Because, the wire is inside the coronary artery there is risk for perforation, which would require surgery to repair. Therefore, this can only be even attempted by someone with a cardiology fellowship followed by 2-3 years of training on top of that for PCI.
The wire has an un-inflated balloon which is inflated once it is directly on top of the thrombosis. The balloon is called an angioplasty balloon. The balloon once deflated, is not enough to keep the region from re-stenosing, so a stent is left in place. The stent can cause problems.
Initially, we used bare metal stents, but the tunica intima saw this the same as plaque and over time it grew over it (called neointimal hyperplasia), creating a stenosis within the stent. Then we used drug eluding stents (DES), which does prevent neointimal hyperplasia but it also increases the risk of thrombosis.
The importance of DAPT in PCI
DAPT or dual antiplatelet therapy is important to prevent thrombosis from occurring after PCI and leading to another ACS episode. The use depends on what was done regarding PCI. If angioplasty balloon alone was used, then DAPT is not needed. If drug eluding stent is used, then 1 year minimum but ideally lifetime of DAPT is needed to prevent the increased risk of thrombosis associated with drug eluding stents. Without this, then patient will likely have thrombosis and another heart attack.
Resources
2019 Canadian Cardiovascular Society/Canadian Association of Interventional Cardiology Guidelines on the Acute Management of ST-Elevation Myocardial Infarction: Focused Update on Regionalization and Reperfusion – link to pdf here.
American Heart Association – EMS Chest pain / ACS guidlines – link here.
Life in the fast lane – Acute Coronary Syndromes article – link here.
Onlinemeded free medical education videos – Acute Coronary syndrome
First10em – Heparin in STEMI and PCI – does it help?
University of Ottawa Heart Institute CODE STEMI protocol – link here.
Alberta Health Services – STEMI Reperfusion order set
Manitoba ACS & STEMI protocol for 2020 – link here (pdf automatically downloads)
Nitroglycerin – Tulane MedWeb
Fibrinolytic therapy for STEMI – ACLS training Center Checklist available here.
Prehospital fibrinolytic Checklist – UNC Medical center- available here.