-
Acute coronary syndromes
Unstable angina & NSTEMI same tx for both. MONABASH + PCTA within 24h. Aspirin + clopidogrel = DAPT (dual antiplatelet therapy), and is a key part. PCTA = PCI. Percutaneous transluminal coronary angioplasty, Percutaneous coronary intervention. MONABASH Monitor Oxygen supplementation if SaO2<90% Nitroglycerin (sublingual) for pain Antiplatelet (aspirin + clopidogrel) Beta-blockers (BBs) — reduce oxygen demand in heart Anticoagulation e.g. UFH, enoxaparin, fondaparinux Statins (High-dose) STEMI stabilize & MONABASH. Reperfusion = PCTA if <90 min, tPA if >120 min eg. IV alteplase. Has to be <12h since symptoms began + IV furosemide if severe pulmonary edema + IV atropine if unstable sinus bradycardia + IV morphine if persistent pain (severe)…
-
Hypertension
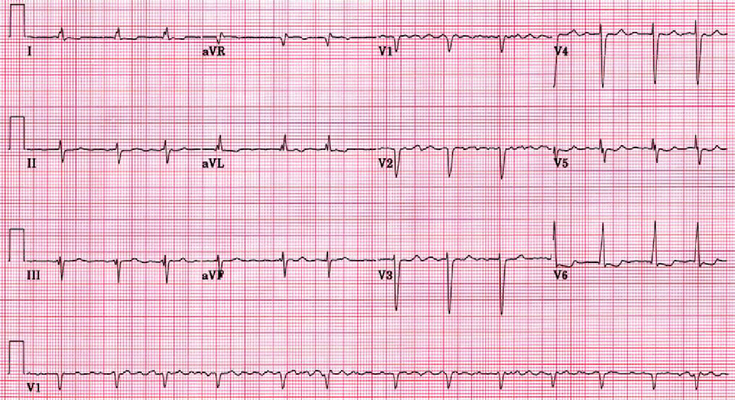
Diagnosis Office BPM ≥180/110 → HTN dx Office BPM ≥140/90 or automated-office BPM ≥135/85 → ambulatory/home BPM to rule out white-coat HTN. If ≥135/85 daytime average or 24h mean ≥130/80 → HTN dx When to start anti-hypertensive drugs? Risk SBP DBP Goal BP (SBP/DBP) on tx Low ≥160 ≥100 <140/90 Mod-high ≥140 ≥90 <140/90 High ≥130 N/A <120/NA DM ≥130 ≥80 <130/80 Routine Lab tests for newly dx HTN Any kidney damage? urinalysis — any hematuria/ proteinuria serum Na, K — RAAS activation serum Cr Any LVH (left-ventricular hypertrophy)? get ECG Any ASCVD risk factors? fasting glucose and/or HbA1c lipid panel: TC, LDL-C, HDL-C, non-HDL-C, TG Pregnancy test before starting…
-
Atrial Fibrillation (Afib)
Acute atrial fibrillation with rapid ventricular rate If patient is experiencing symptoms get an IV placed and cardiac monitoring started If the patient is hemodynamically unstable give them synchronized cardioversion with rapid ventricular rate the goal is to get the heart rate below 110 bpm, and this is done with rate control medications. Find out if they have heart failure (acute decompensated heart failure) – if yes, then they will usually get digoxin or amiodarone. If no, then a calcium channel blocker like diltiazem or a beta-blocker like metoprolol If they received electrical cardioversion they will need anticoagulation for 1 month Chronic Atrial fibrillation Rate and Rhythm control have similar…
-
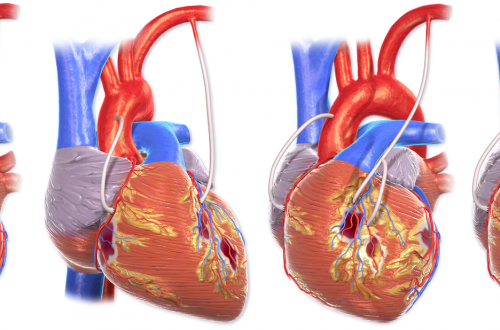
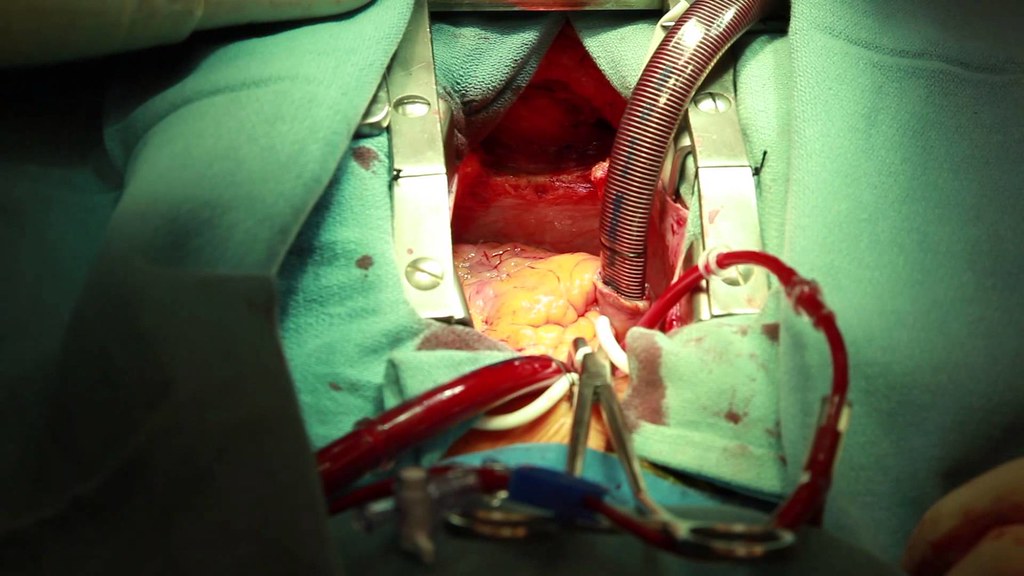
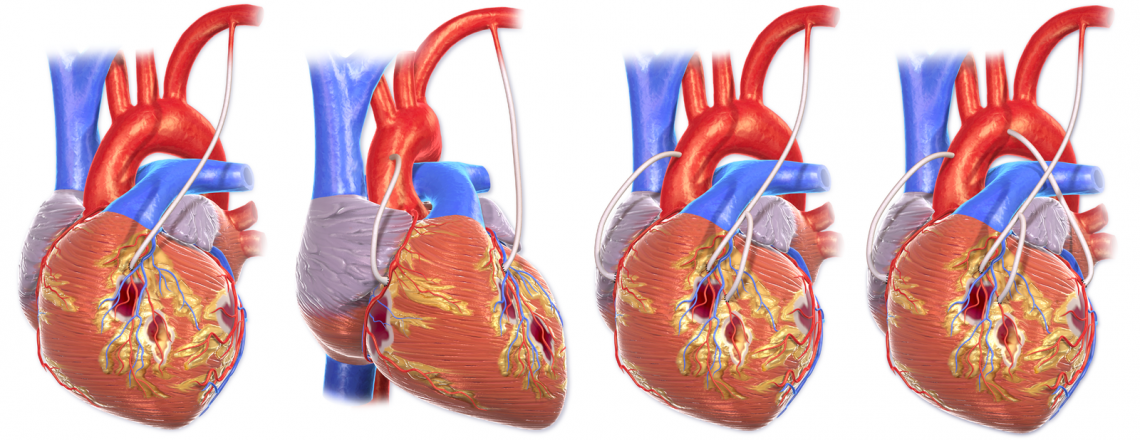
Coronary Artery Bypass Grafting
The goal of CABG is to restore blood flow to the myocardium. Preoperative Care During preoperative assessment of patients undergoing coronary artery bypass grafting, special care should be paid to the severity of their coronary artery disease, their vascular function, the presence of comorbid disease, and explaining to the patient the procedure and postoperative care expectations. Medications Cardiac medications are to be continued up to the morning of the operation, except ACE inhibitors and digoxin. Monitoring Routine monitoring of CABG patients often includes: 5 lead ECG Temperature – core temperature (nasopharyngeal) Pulse oxymetry Capnography Central venous pressure Invasive BP monitoring Anesthesia for CABG An example protocol for induction: Etomidate, Fentanyl,…
-
Chest Pain
Intravenous Fluid Orders Intravenous Cannula – Insert IV Peripheral Saline Flush/Lock: Saline Lock IV Maintenance: 0.9% NaCl infusion at ______ mL/hour, reassess after hours lactated ringers infusion at ______ mL/hour, reassess after hours IV Bolus: 0.9% NaCl ______ mL over ______ hour(s) lactated ringers _______ mL over _______ hour(s) Laboratory Investigations Hematology Complete Blood Count (CBC) PT INR Chemistry Troponin Repeat Troponin_________time(s) (specify collection time below) ___________:_____________ ___________:_____________ Electrolytes (Na, K, Cl, CO2) Glucose Creatinine Urea Serum bHCG Urine Tests Urine Dipstick Testing – POCT Urinalysis Pregnancy Test, Urine (POCT if available) Other Labs (based on presentation needs of the patient) Diagnostic Imaging Chest x-ray usually indicated unless recently performed to rule out…
-
Acute Coronary Syndromes
Checklist ECG: Get a 12 lead ECG within 10 minutes of patient presenting with chest pain Vitals: Take initial vital signs: temp, HR, RR, SpO2, BP in both arms; and repeat if there further chest pain or equivalent symptoms Oxygen: Give Oxygen if SpO2 ≤ 90% or there are clinical signs of hypoxemia Antiplatelets: Give acetylsalicylic acid (Aspirin®) now if it was not given prior to arrival at hospital. Write down when it was given. Nitroglycerin: Give Nitroglycerin in hemodynamically stable patients every 5 minutes as needed. *Avoid if suspected RV infarction. Dose: usually 0.3 to 0.4 mg. Place defibrillation pads on chest – because there is a high risk…