Hypertension
Diagnosis
- Office BPM ≥180/110 → HTN dx
- Office BPM ≥140/90 or automated-office BPM ≥135/85 → ambulatory/home BPM to rule out white-coat HTN. If ≥135/85 daytime average or 24h mean ≥130/80 → HTN dx
When to start anti-hypertensive drugs?
| Risk | SBP | DBP | Goal BP (SBP/DBP) on tx |
| Low | ≥160 | ≥100 | <140/90 |
| Mod-high | ≥140 | ≥90 | <140/90 |
| High | ≥130 | N/A | <120/NA |
| DM | ≥130 | ≥80 | <130/80 |
Routine Lab tests for newly dx HTN
- Any kidney damage?
- urinalysis — any hematuria/ proteinuria
- serum Na, K — RAAS activation
- serum Cr
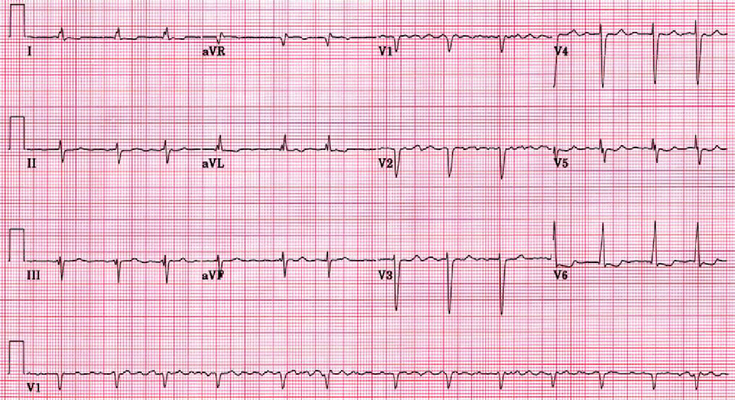
- Any LVH (left-ventricular hypertrophy)? get ECG
- Any ASCVD risk factors?
- fasting glucose and/or HbA1c
- lipid panel: TC, LDL-C, HDL-C, non-HDL-C, TG
- Pregnancy test before starting therapy
Lifestyle Modification
Same for all the “lifestyle diseases”
- Weight loss is #1 most effective therapy if obese
- DASH/ Mediterranean diet
- Regular exercise: aerobic & resistance
- Goal is BMI <25, waist <102 cm (male), <88 cm (female)
- Stop smoking
- No alcohol or limited amount
Choice of antihypertensive
depends on comorbidities, pregnancy, etc
| Condition | Drug choice | Avoid |
| pregnant/ desiring to be pregnant | ER* Nifedipine Labetalol** Hydralazine (2nd line) Methyldopa *extended release (never use short-acting version for HTN tx) | RAAS drugs (ACEI/ ARB/ MRA) Nitroprusside Labetalol (avoid if asthma/ severe bradycardia) |
| Lactation | ER Nifedipine Labetalol Enalapril/ Captopril | |
| Gout | Losartan or other ARBs CCBs | Diuretics |
| Osteoporosis | Thiazides | |
| Angina pectoris | BBs CCBs | |
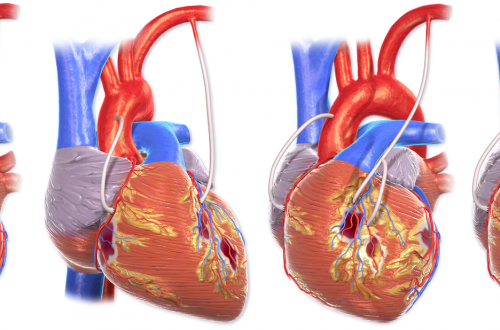
| Post-MI | ACEI/ ARB BBs | avoid CCBs if heart failure |
| HFrEF | ACEI/ ARB/ BB/ Aldosterone agonist Diuretic | |
| Afib/ AF | BB non-dihydropyridine CCB | |
| CKD | BB non-dihydropyridine CCB | |
| Migraine | BB or CCB | |
| Diabetes Mellitus | ACEI/ ARB CCB | Thiazides Older beta-blockers (PAM**) |
| LVH | ACEI/ ARB CCB/ Thiazides | Hydralazine minoxidil |
| TIA/ Stroke | ACEI + Thiazide combo | |
| Peripheral artery disease | any choice | beta-blockers if severe disease |
| Older adult (>60 y) | beta-blockers | |
| African descent | ACEIs unless diabetic | |
**PAM (propranolol, atenolol, metoprolol) are older beta-blockers that only have beta-1 inhibitor activity leading to unopposed alpha-1 activity → hyperglycemia and in atenolol & metoprolol → ↑vasoconstriction. Avoid if diabetic
Notes:
- usually bad to combine ACEI with ARB
Secondary Hypertension
| Cause | Dx/Tx | |
| Hyperaldosteronism | hypokalemia is a key clue | ↑BP with ↓K+ *see image below for diagnostic tests * |
| Obstructive sleep apnea (OSA) | relaxation of pharyngeal muscles –> closure of airway. Men with obesity @ highest risk. Loud snoring, periods of apnea, daytime sleepiness, HTN, pulm HTN, right sided HF due to apnea triggering stress (catecholamine) response. Also can lead to CAD & Afib | |
| Oral contraceptives | ~5% of chronic users can get overt HTN. May be due to estrogen-induced liver synthesis of angiotensinogen | switch to alternative contraception eg copper-IUD |
| Cocaine | epistaxis, termor, ↑HR, ↑BP, usually young, get urine drug screen | |
| Fibromuscular dysplasia (FMD) | 90% of patients are women secondary hyperaldosteronism (↑renin –> ↑aldosterone) due to vessel stenosis (non-atherosclerotic, non-inflammatory; due to abnormal cell development). Multiple arteries (internal carotid, renal, abdominal aorta) | CT angiogram if abdomen/ Duplex US, and if negative, get catheter based digital subtraction arteriography. ACEI/ARB (1st line), PTA (percutaneous transluminal angiography) or surgery. Follow-up: BP & Cr q3-4 months, renal US q6-12 mo. |
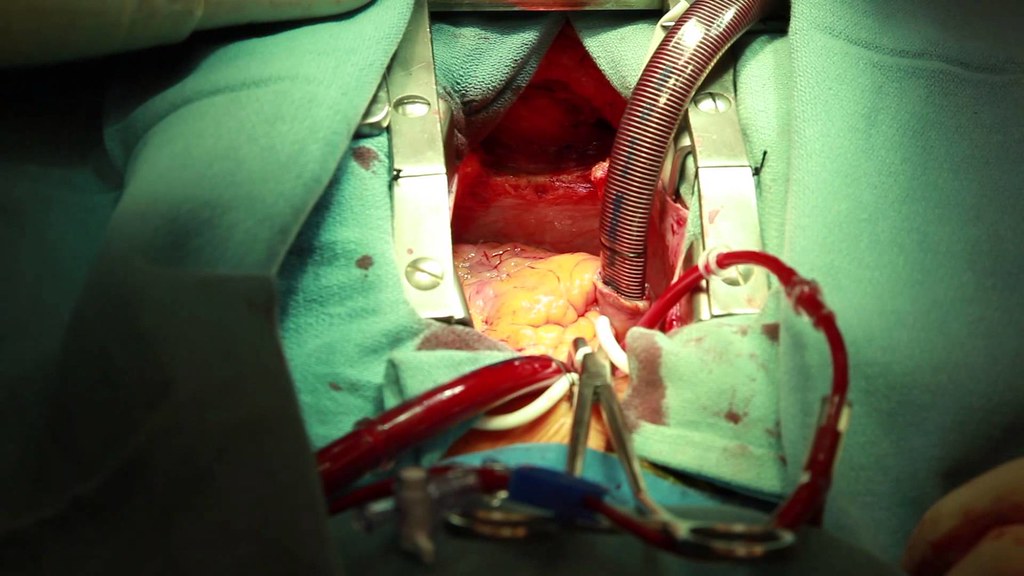
| Renal artery stenosis (renovascular disease) | Severe HTN (>180/120) after age 55. Recurrent flash pulmonary edema (normal EF so not CHF). Abdominal bruit, asymmetric (one small) kidneys. Usually has severe atherosclerosis. | renal doppler US ACEI/ARB (1st choice, monitor Cr because 30% develop ↑Cr) Revascularization Atherosclerosis risk reduction (statins, stop smoking) |
| Pheochromocytoma | classic triad: episodic headache, sweating & tachycardia Resistant HTN or HTN with ↑glucose. Family Hx or familial syndrome (MEN2, NF1, VH2). 10% bilateral, 10% extra-adrenal, 10% malignant. Neuroendocrine tumor from chromaffin cells → release catecholamines (D, EPI, NE) which break down into metanephrines (↑ in urine/ plasma). | Confirm with abdominal CT scan. Pre-op adrenergic blockade (alpha blocker first then beta-blocker). eg phenoxybenzamine or tetrazosin started 7-14 d pre-op then propranolol started 2-3 d pre-op. Laparoscopic/ open resection of tumor (s) |
| Thyroid disease | Hyperthyroidism Hypothyroidism | |
| Primary hyperparathyroidism | ↑Ca Bones, groans, (kidney) stones, psychic overtones (depressed, poor sleep) 80% due to parathyroid adenoma | |
| ADPKD | 30-40 year old HTN + flank pain, hematuria, palpable, abdominal masses. PKD1 or PKD2 mutations (code for polycystins — aneurysms in kidney and other locations eg hepatic/ aortal/ colon/ hernias) | Abdominal US (multiple renal cysts) ACEI Hemodialysis/ renal transplant for ESRD |
| Pre-eclampsia | Low-dose aspirin* delivery @ ≥37 weeks supplemental calcium if needed Exercise & weight loss if needed Goal DBP ≤85 *from before 16 wks to 36 wks to reduce risk in high-risk women | |
| Eclampsia | MgSO4 (1st choice) |