Coronary Artery Bypass Grafting
The goal of CABG is to restore blood flow to the myocardium.
Preoperative Care
During preoperative assessment of patients undergoing coronary artery bypass grafting, special care should be paid to the severity of their coronary artery disease, their vascular function, the presence of comorbid disease, and explaining to the patient the procedure and postoperative care expectations.
Medications
Cardiac medications are to be continued up to the morning of the operation, except ACE inhibitors and digoxin.
Monitoring
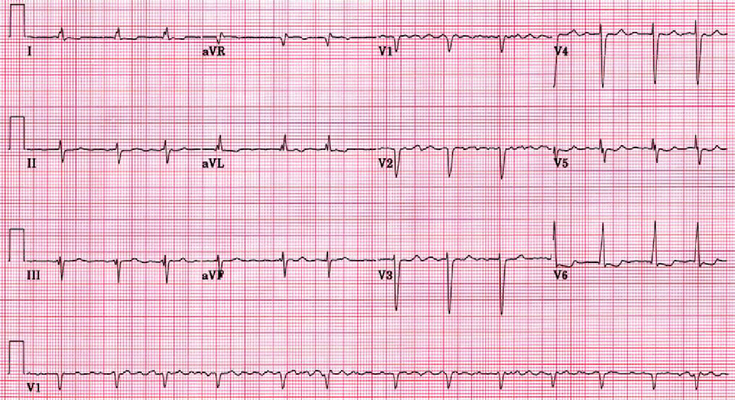
Routine monitoring of CABG patients often includes:
5 lead ECG
Temperature – core temperature (nasopharyngeal)
Pulse oxymetry
Capnography
Central venous pressure
Invasive BP monitoring
Anesthesia for CABG
An example protocol for induction: Etomidate, Fentanyl, and Rocuronium (muscle relaxant). For maintanence: an inhalational agent e.g. isoflurane or an infusion of propofol.
CABG operation
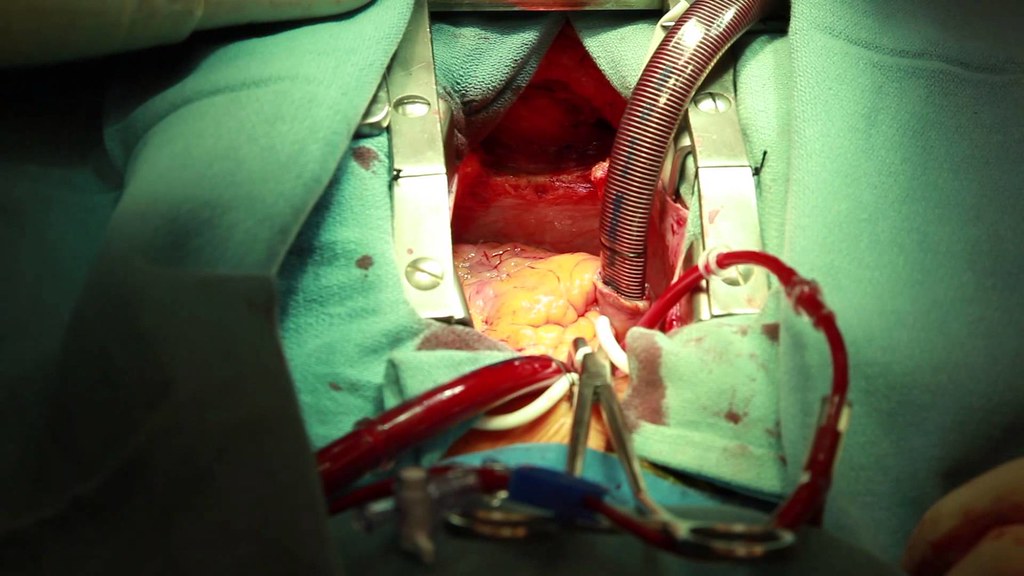
Coronary artery bypass grafting is an invasive procedure that require the chest to be opened. This is usually done by median sternotomy or another thoracotomy incision, and then the pericardium is incised. Caridopulmonary bypass (CBP) may be used and is stopped after the conduit has been grafted/ attached. The pericardium is left open until the patient is hemodynamically stabilized after which a closed water-seal chest drain is applied and the wound is closed.
Postoperative Care
Cardiovascular post-op complications include: hypotension (due to low CO or low SVR), hypertension, arrhythmias, conduction abnormalities and pulmonary hypertension.
Respiratory complications following CABG include atelectasis, penumothorax, hydrothorax, bronchospasm, and failure to wean from ventilator.
Conduits for CABG
Internal Mammary Arteries (aka Internal Thoracic Arteries as conduits
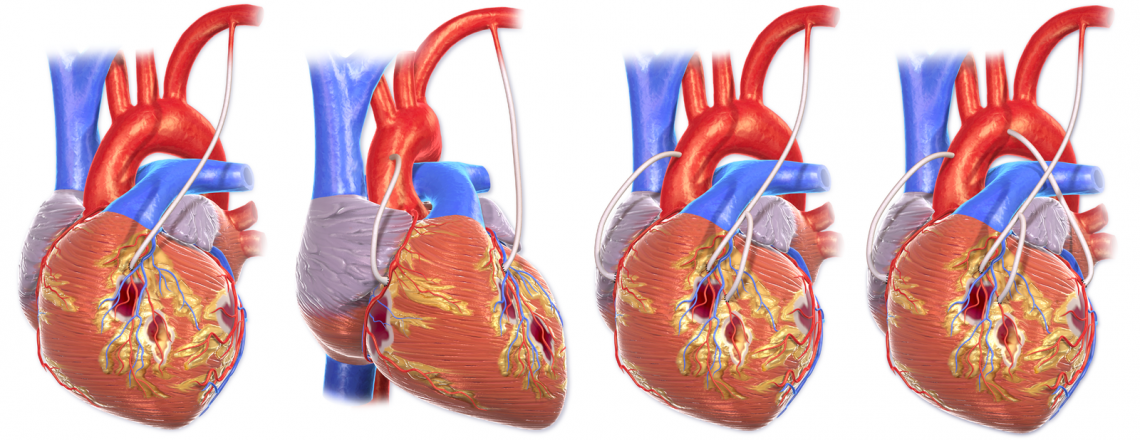
The internal mammary arteries, also called the internal thoracic arteries, are the most commonly used vessels for coronary artery bypass grafting. This is because of their excellent long term patency. Both the left and right internal mammary arteries have a patency greater than 90%, usually said to be 95%, at 15 years post operation.
The left internal mammary artery (LIMA) is the most commonly used source for grafting aka conduit. When right internal mammary artery (RIMA) is also used in addition to LIMA when bilateral grafts are needed. However, this can increase the risk of the sternum not healing properly. The RIMA is often used for occlusion of the right coronary artery (RCA), whereas the LIMA is often used for occlusion of the left anterior descending artery (LAD) as well as occlusion of the diagonal branch of the LAD and the left circumflex artery (LCX).
During harvesting, the entire LIMA is removed with only a small amount of tissue left at its origin at the subclavian artery. When grafted onto the LAD, the anastomosis is done either side-to-side or end-to-side.
Saphenous Veins as conduits
When multiple vessels are occluded/ severely stenosed, then the greater saphenous and lesser saphenous veins can be used. However, it has a lower patency rate long term, and is not an option in patients with venous insufficiency, arterial insufficiency or deep vein thrombosis because of concerns over healing of the harvesting site.
The gastroepiploic, inferior epigastric, and radial arteries are sometimes used as free grafts. Lastly, when there is no other conduit available, cryopreserved saphenous veins or umbilical vein allografts may be used, but they are last choice because of their poor patency.
Conduits (graft sources) for CABG
| Graft source (conduit) | Details |
|---|---|
| Left Internal Mammary Artery (LIMA) | Best option with 95% patency rate at 15 years |
| Saphenous Veins | 25% patency at 10 years, 50% occluded, 25% stenosed |
| Right Internal Mammary Artery (RIMA) | Similar patency rate to LIMA, used when both arteries are needed |
| Radial Artery | Risk of severe post-op vasospasm; patency 90% at 5 years |
| Right Gastroepiploic Artery | 90% patency at 5 years; use limited because artery is fragile, and technical issues |
| Inferior epigastric artery |
Resources
Cover image from: Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014“.
WikiJournal of Medicine 1 (2).