-
Acute coronary syndromes
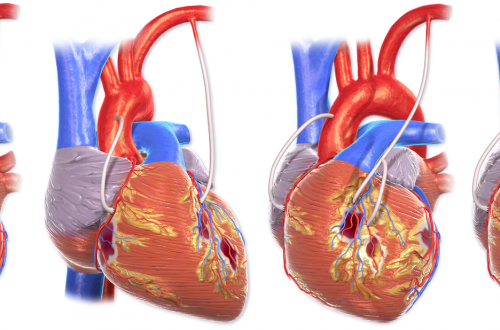
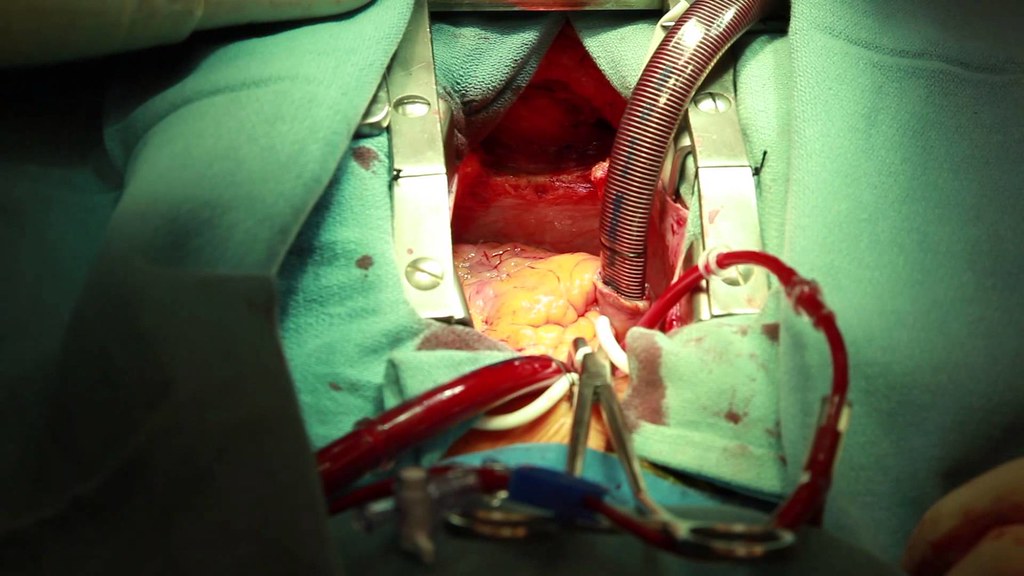
Unstable angina & NSTEMI same tx for both. MONABASH + PCTA within 24h. Aspirin + clopidogrel = DAPT (dual antiplatelet therapy), and is a key part. PCTA = PCI. Percutaneous transluminal coronary angioplasty, Percutaneous coronary intervention. MONABASH Monitor Oxygen supplementation if SaO2<90% Nitroglycerin (sublingual) for pain Antiplatelet (aspirin + clopidogrel) Beta-blockers (BBs) — reduce oxygen demand in heart Anticoagulation e.g. UFH, enoxaparin, fondaparinux Statins (High-dose) STEMI stabilize & MONABASH. Reperfusion = PCTA if <90 min, tPA if >120 min eg. IV alteplase. Has to be <12h since symptoms began + IV furosemide if severe pulmonary edema + IV atropine if unstable sinus bradycardia + IV morphine if persistent pain (severe)…
-
Hypertension
Diagnosis Office BPM ≥180/110 → HTN dx Office BPM ≥140/90 or automated-office BPM ≥135/85 → ambulatory/home BPM to rule out white-coat HTN. If ≥135/85 daytime average or 24h mean ≥130/80 → HTN dx When to start anti-hypertensive drugs? Risk SBP DBP Goal BP (SBP/DBP) on tx Low ≥160 ≥100 <140/90 Mod-high ≥140 ≥90 <140/90 High ≥130 N/A <120/NA DM ≥130 ≥80 <130/80 Routine Lab tests for newly dx HTN Any kidney damage? urinalysis — any hematuria/ proteinuria serum Na, K — RAAS activation serum Cr Any LVH (left-ventricular hypertrophy)? get ECG Any ASCVD risk factors? fasting glucose and/or HbA1c lipid panel: TC, LDL-C, HDL-C, non-HDL-C, TG Pregnancy test before starting…
-
Thrombocytopenia
Condition Notes ITP due to antibodies made after viral infection.mucocutaneous bleeding (epistaxis, hematuria, ecchymosis, petechiae) ↓PLT↑BT (normal PT & PTT)normal/ slightly ↑ size observe only if mild (cutaneous bleeds, PLT ≥30,000)Steroids/IVG/anti-D if severe (bleeding or PLT<30,000)Test for HCV & HIV TTP hereditary/ acquiredAntibody against ADAMTS13 → uncleared vWF multimers → PLT trapping & activationfever, neuro sx, renal failure ↓PLT with hemolysis (↑LDH, ↓haptoglobin, ↓RBC, schistocytes)↑BT (normal PT & PTT) plasma exchange/ steroids/ rituximabreplenishes ADAMTS13 & removes antibodies HIT-1 heparin activates PLT directly → ↓PLT count within the first 2 days of use. Then PLT normalizes. Milder than HIT-2 HIT-2 auto-immune: antibodies against PLT factor 4 (PF4) complex with heparin. Seen…
-
Blood Transfusion Reactions
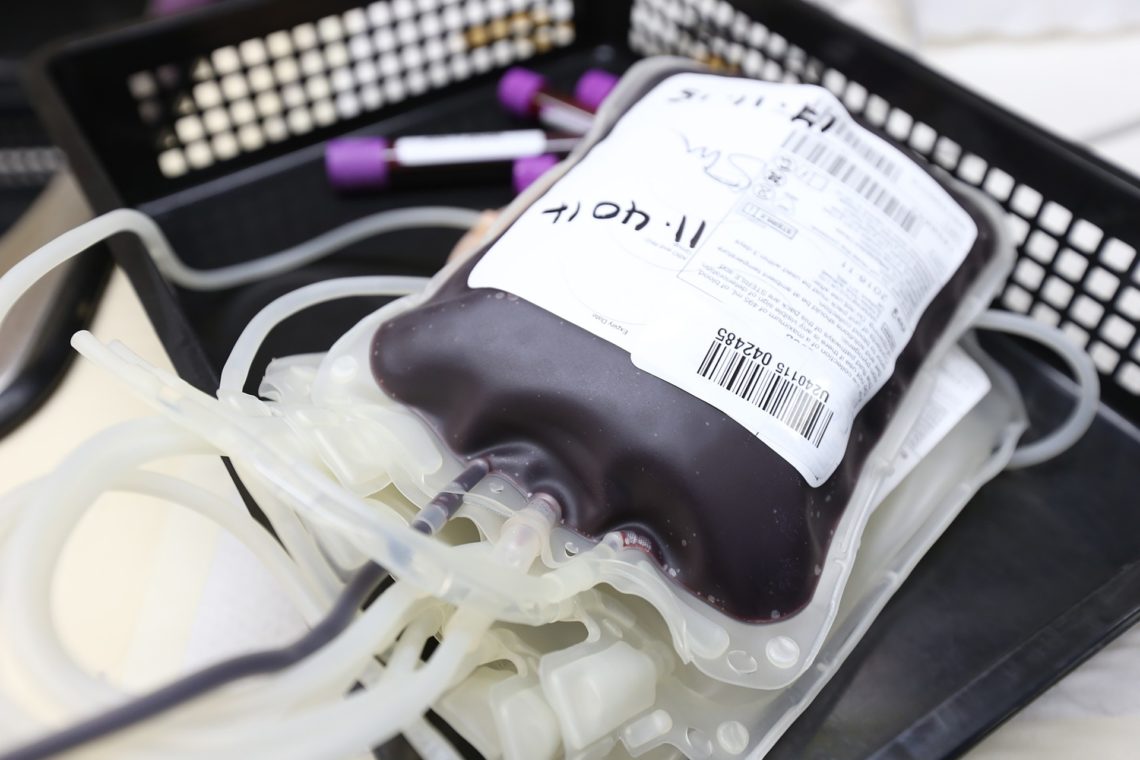
Type Tx Anaphylactic ImmediateIgA deficiencyAngioedema Stop transfusionIM Epi +/- Bronchodilators/ antihistamine Acute hemorrhagic <1hABO incompatibility+Coombsflank pain, fever, hemoglobinuria, DIC Stop transfusionIVF, supportive care Febrile non-hemolytic 1-6hfever, chills Stop transfusionAntipyreticsPrevention: filter out WBC (leuko-reduction) Urticarial 2-3hIgE Stop transfusionAntihistamine (eg diphenhydramine) Transfusion-related acute lung injury (TRALI) <6hdonor anti-leukocyte antibodiesResp. distress, pulmonary edema Stop transfusionSupportive care (may need ventilator)50% die, rest better in 1-2 days Delayed hemolytic days-weeks laterAnamesic antibody+Coombs, +Ab screenasymptomatic Graft vs Host <weeksDonor T lymphocytesPancytopenia, GI Sx, rash, fever Steroids Bacterial Sepsis min-hoursfever, shock, DIC
-
Aphasia
Terminology Dysarthria = problem with slurring of speech Articulation defects = problems with motor control of the mouth Anomia = inability to name things, a key finding in almost all aphasias. Mild anomia is difficulty naming objects that are less commonly used in speech. Severe anomia is difficulty naming everyday objects. Anosognosia = person is unaware that they have a neurologic deficit, typically due to a lesion in the non-dominant hemisphere Apraxia = person is unable to carry out a learned motor task but their motor, sensory and coordination is preserved – so they should be able to perform the task. Agnosia = person is unable to recognize objects Prosopagnosia…
-
Nervous System Hemorrhage
Extraparenchymal –> outside of brain Caput succedaneum = blood above the glea aproneurotica but under the scalp Subgleal hemorrhage = blood under the glea aproneurotica and between the skull opening Cephalohematoma = blood under the upper periosteum and above the skull Epidural hematoma = blood under the lower periosteum and above the dura mater Subdural hematoma = blood under the dura mater and in the arachnoid/ above the pia mater. Intraparenchymal –> into brain Subarachnoid hemorrhage = bleeding under the arachnoid membrane but above the pia mater. Cerebral lobe (cortical) hemorrhage = bleeding can be in the dominant and non-dominant frontal lobes, parietal lobes, and temporal lobes or the occipital…
-
Intraventricular Hemorrhage
The germinal matrix is a region in the developing fetus that is located next to the ventricles (periventricular) and gives rise to neurons and glial cells. It is highly vascularized with fragile capillaries that can easily rupture. This region involutes by 32 weeks of gestation. There is supporting structures around it that develop and protect it. In premature babies born before 32 weeks, the germinal matrix has not involuted putting them at risk for rupture of the fragile capillaries leading to intraventricular hemorrhage (IVH). In very low birth weight newborns, <1500g, the risk of germinal matrix capillary rupture is also increased. The blood coagulates and can be easily visualized with…
-
Anterior Pituitary Disorders
Name 7 disorders of the anterior pituitary? Remember anterior pituitary produces FLAT PiG (FSH, LH, ACTH, TSH, Prolactin, GH) so in that order… FSH or LSH producing tumors – called functional gonadotroph adenomas (FGA) ACTH producing adenoma – Cushing’s disease TSH producing adenoma – Central hyperthyroidism Prolactin producing adenoma (prolactinoma) GH producing adenoma (gigantism in kids, acromegaly in adults) Hypopituitarism – can be due to infection, infarction, or surgery. Acute hypopituitarism can lead to coma and death. Empty Sella syndrome – pituitary is located elsewhere rather than in the sell turcica, so not seen there on MRI. What are 4 expected symptoms & signs for hyperprolactinemia? Hypogonadism – in women…
-
Alzheimer Disease
Alzheimer’s disease is the most common cause of dementia (now called major neurocognitive disorder) affecting as many as 5.8 million Americans in 2020 and this number is expected to triple to nearly 14 million by 2060. Pathophysiology of Alzheimer’s Disease Alzheimer’s disease is a neurodegenerative condition that occurs as a result of a buildup of amyloid protein in beta-pleated sheets along with tau protein. Pathology will reveal neuritic plaques, neurofibrillary tangles of tau protein, and extra-cellular deposition of amyloid beta-proteins. The brain in Alzheimer’s disease shows several changes including enlargement of ventricles, shrinkage of cerebral cortex and shrinkage of the hippocampus. One area of the brain that degenerates in Alzheimer’s…
-
Memory Disorders
Terminology Declarative memory: Semantic declarative memory:remembering facts e.g. numbers and areas of knowledge e.g. language Episodic declarative memory: remembering the time and place Procedural memory: remembering how to do things e.g. ride a bicycle Short term memory: recent memory of events e.g. what you had for breakfast Immediate short term memory: Being able to recall a fact just told to you e.g. repeat the following phone number. Long term memory: remembering something from your childhood Aphasia: impaired language/ communication. Expressive aphasia (Broca’s): impaired language fluency, and repetition, normal comprehension Receptive aphasia (Wernicke): impaired comprehension and repetition but normal fluency. Conduction aphasia: impaired repetition but normal comprehension and fluency. Global aphasia:…