-
OBGYN: infections
Urinary tract infections Antibiotics for UTIs Ceftriaxone [Rocephin®] (IV) — used for hospitalized patients to treat pyelonephritis. Always hospitalize pregnant women with pyelonephritis. After 2 days of no fever (clinical improvement) can switch to oral medication to continue treating pyelonephritis. Remember, pyelonephritis requires 5-14 days of antibiotics to eliminate bacteria from the entire urinary tract (kidney, renal collecting ducts, bladder). Cephalexin [Alcephin®, Keflex®] (oral) — safe in pregnancy. Fosfomycin [Monuril®] (oral) — safe in pregnancy Nitrofurantoin (oral) — used for cystitis only, does not achieve enough concentration in kidneys to treat pyelonephritis. Trimethoprim-sulfamethoxazole [Bactrim®] (oral) — used for cystitis only, does not achieve enough concentration in kidneys to treat pyelonephritis.…
-
Obstetrics: intrapartum care
these are personal notes only not meant for other uses. True labor vs false labor False labor: uterine contractions are not regular and do not result in cervical change. Also called “Braxton-Hicks” contractions True labor: regular uterine contracts that result in progressive cervical dilation and effacement. True labor is likely if painful contractions every 5 minutes for 1 hour. Stages & Phases of labor Stage 1: from onset of true labor to full cervical dilation (10cm). It has 2 phases: Latent phase: from onset of labor to period of rapid dilation (1-2cm/h). Active phase: from the period of rapid dilation (typically at 6cm dilation is when it speeds up ~1-2cm/h;…
-
Obstetrics: Physiology
A pregnant woman complains of increased urination, and has +2 glucose on urine dipstick. Pregnant women are more likely to get diabetes because human placental lactogen (hPL) reduces the response to insulin, to allow for a more constant supply of glucose to the fetus. However, finding glucose on urine dipstick can be normal, because during pregnancy there is increased blood flow to the kidneys and increased glomerular filtration rate (GFR). More filtration (high GFR) results in more glucose in the urine. Increased renal blood flow, results in increased urine output and along with compression of the bladder by the growing uterus, this often leads to increased urination. A pregnant woman…
-
Acute coronary syndromes
Unstable angina & NSTEMI same tx for both. MONABASH + PCTA within 24h. Aspirin + clopidogrel = DAPT (dual antiplatelet therapy), and is a key part. PCTA = PCI. Percutaneous transluminal coronary angioplasty, Percutaneous coronary intervention. MONABASH Monitor Oxygen supplementation if SaO2<90% Nitroglycerin (sublingual) for pain Antiplatelet (aspirin + clopidogrel) Beta-blockers (BBs) — reduce oxygen demand in heart Anticoagulation e.g. UFH, enoxaparin, fondaparinux Statins (High-dose) STEMI stabilize & MONABASH. Reperfusion = PCTA if <90 min, tPA if >120 min eg. IV alteplase. Has to be <12h since symptoms began + IV furosemide if severe pulmonary edema + IV atropine if unstable sinus bradycardia + IV morphine if persistent pain (severe)…
-
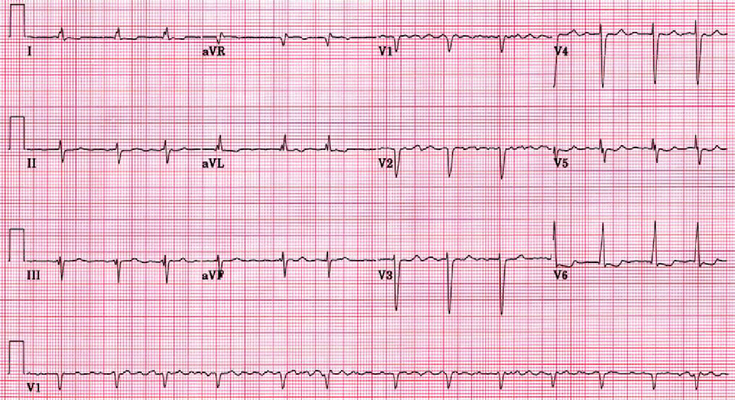
Hypertension
Diagnosis Office BPM ≥180/110 → HTN dx Office BPM ≥140/90 or automated-office BPM ≥135/85 → ambulatory/home BPM to rule out white-coat HTN. If ≥135/85 daytime average or 24h mean ≥130/80 → HTN dx When to start anti-hypertensive drugs? Risk SBP DBP Goal BP (SBP/DBP) on tx Low ≥160 ≥100 <140/90 Mod-high ≥140 ≥90 <140/90 High ≥130 N/A <120/NA DM ≥130 ≥80 <130/80 Routine Lab tests for newly dx HTN Any kidney damage? urinalysis — any hematuria/ proteinuria serum Na, K — RAAS activation serum Cr Any LVH (left-ventricular hypertrophy)? get ECG Any ASCVD risk factors? fasting glucose and/or HbA1c lipid panel: TC, LDL-C, HDL-C, non-HDL-C, TG Pregnancy test before starting…
-
Thrombocytopenia
Condition Notes ITP due to antibodies made after viral infection.mucocutaneous bleeding (epistaxis, hematuria, ecchymosis, petechiae) ↓PLT↑BT (normal PT & PTT)normal/ slightly ↑ size observe only if mild (cutaneous bleeds, PLT ≥30,000)Steroids/IVG/anti-D if severe (bleeding or PLT<30,000)Test for HCV & HIV TTP hereditary/ acquiredAntibody against ADAMTS13 → uncleared vWF multimers → PLT trapping & activationfever, neuro sx, renal failure ↓PLT with hemolysis (↑LDH, ↓haptoglobin, ↓RBC, schistocytes)↑BT (normal PT & PTT) plasma exchange/ steroids/ rituximabreplenishes ADAMTS13 & removes antibodies HIT-1 heparin activates PLT directly → ↓PLT count within the first 2 days of use. Then PLT normalizes. Milder than HIT-2 HIT-2 auto-immune: antibodies against PLT factor 4 (PF4) complex with heparin. Seen…
-
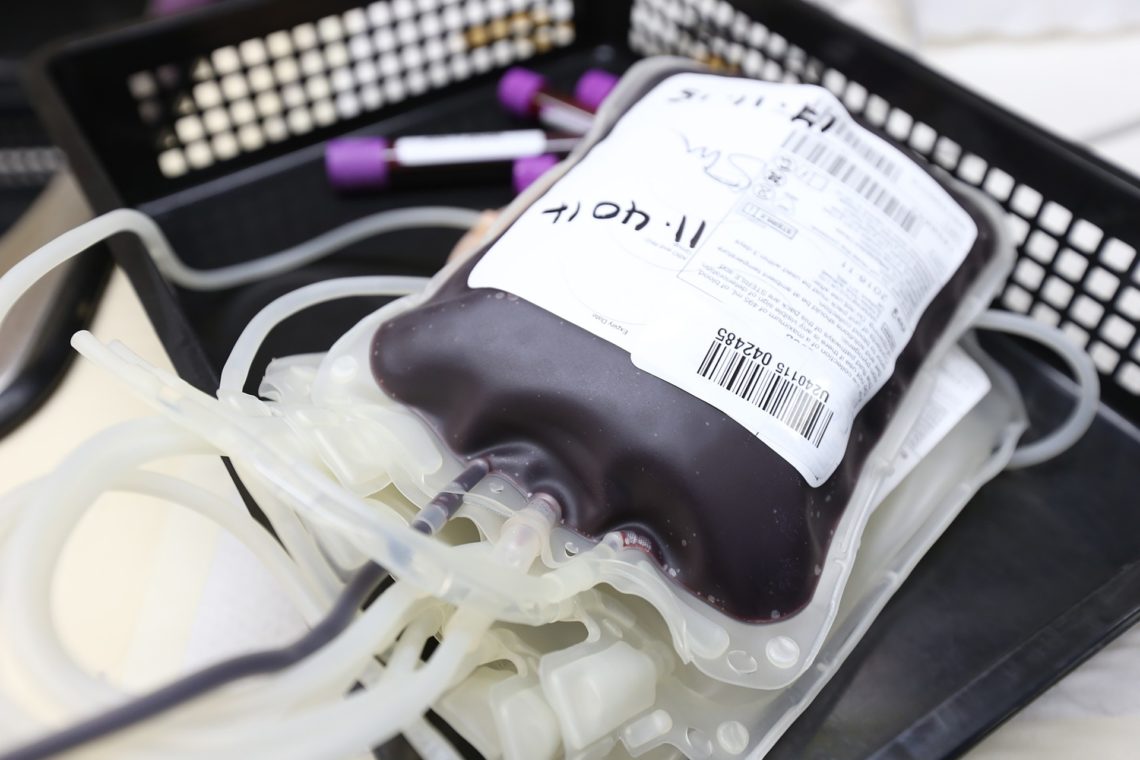
Blood Transfusion Reactions
Type Tx Anaphylactic ImmediateIgA deficiencyAngioedema Stop transfusionIM Epi +/- Bronchodilators/ antihistamine Acute hemorrhagic <1hABO incompatibility+Coombsflank pain, fever, hemoglobinuria, DIC Stop transfusionIVF, supportive care Febrile non-hemolytic 1-6hfever, chills Stop transfusionAntipyreticsPrevention: filter out WBC (leuko-reduction) Urticarial 2-3hIgE Stop transfusionAntihistamine (eg diphenhydramine) Transfusion-related acute lung injury (TRALI) <6hdonor anti-leukocyte antibodiesResp. distress, pulmonary edema Stop transfusionSupportive care (may need ventilator)50% die, rest better in 1-2 days Delayed hemolytic days-weeks laterAnamesic antibody+Coombs, +Ab screenasymptomatic Graft vs Host <weeksDonor T lymphocytesPancytopenia, GI Sx, rash, fever Steroids Bacterial Sepsis min-hoursfever, shock, DIC
-
CTFPHC guidelines summary
for low risk / general population — see Canadian Task Force on Preventative Health Care website for the guidelines, below is only a summary table for educational purposes only. Screen for Age Test Do not use... Breast cancer (2018) *to be updated in fall 2023 50-74 mammogram q2-3y MRI/US/clinical or self breast exam Colorectal cancer 50-74 FOBT (gFOBT/FIT) q2-3y or flexible sigmoidoscopy q10y colonoscopy — done if pt. has sx (eg bleeding) Lung cancer 55-74 with ≥30 pack-year smoking who currently smoke or quit <15y ago. (e.g. 2 packs/day x 15y = 30 pack-years) Low-dose CT annually upto 3 consecutive times CXR Cervical cancer 25-69 stop @70 if last 3…
-
Pregnancy Screening & Testing
First prenatal visit Blood type & Rh FactorRubella IgG and IgM — positive IgG only = immuneCBCHBsAgVDRL (syphilis) — can use EIA Ab then RPR. Re-screen @ deliveryHIV antibodySTI (chlamydia, gonorrhea) — with NAATVaricella IgG — (+) means immuneSafe vaccines = Tdap, flu, HBVUnsafe vaccines = HPV, MMR, Varicella, live attenuated influenzaDiclectin® (pyridoxine/doxylamine) for nausea/vomiting Second prenatal visit PAP smear if not done in last 3 years Week 11 Dating ultrasound @ 8-12 weeksWeek 11-14: Beta-hCG, PAPP-A, nuchal translucencyWeek 15-20: MSAFP, Beta-hCG, estrogen, inhibin AChorionic villus sampling (week 10), amniocentesis (week 15) Week 20 Ultrasound anatomy scan offered Week 24-28 Tdap @ 27-32 weeks Week 35-37 GBS swab Week 38-39…
-
Types of Research Studies
Experimental studies: Randomized control trial (RCT) can determine efficacy of treatmentrandom Non-random study Observational studies: Cohort study risk factors/ outcomeslongitudinalincidence Cross-sectional study prevalencesnapshotassoc. between risk factors & diseaseused to generate hypothesis (Ho) & sometimes to test Ho Case-control study cases (disease positive) compared to controls (disease negative)looks at odds of exposure Case report series one person or small group of people detailed info used to generate Ho Reviews: Meta-analysis data from multiple studies combined and analyzed Systematic reviews Experts: Expert opinions & panels Grades of evidence in research studies Meta-analysis and systemic reviews are the research studies with the best evidence, grade 1 evidence. Randomized control trials follow closely, then…