Obstetrics: intrapartum care
these are personal notes only not meant for other uses.
True labor vs false labor
- False labor: uterine contractions are not regular and do not result in cervical change. Also called “Braxton-Hicks” contractions
- True labor: regular uterine contracts that result in progressive cervical dilation and effacement. True labor is likely if painful contractions every 5 minutes for 1 hour.
Stages & Phases of labor
Stage 1: from onset of true labor to full cervical dilation (10cm). It has 2 phases:
- Latent phase: from onset of labor to period of rapid dilation (1-2cm/h).
- Active phase: from the period of rapid dilation (typically at 6cm dilation is when it speeds up ~1-2cm/h; nulliparous women ~1.2cm/h and multiparous women ~1.5cm/h) until fully dilated. Rapid dilation (active phase) starts typically when the cervix is dilated to 4cm in ~60% of women and 6cm in ~90% of women.
Stage 2: from full cervical dilation (10 cm) to delivery of the infant
Stage 3: from delivery of the infant to delivery of the placenta. Can take up to 30 minutes.
Stage 4: from delivery of the placenta to 2 hours later. Also called the immediate postpartum period
Duration: for 1st vaginal delivery it takes ~2-3 hours; for multiparous women it takes less time. Delivery is imminent when a coin sized amount of the fetal head is visible.
Cardinal movements of labor
EDFIrEErE: Engagement, Descent, Flexion, Internal rotation, Extension, External rotation, Expulsion.

Delivery of the Newborn
Stage 2 of Labor
Delivery of the head: Delivery is imminent when there is a coin sized amount of the fetal head visible. First support the perineum and the fetal head as it comes out in extension. After delivery of the head there is restitution.
Delivery of the anterior shoulder. If the anterior shoulder is stuck it is called shoulder dystocia. Anterior shoulder is caught behind the pubic sypmphysis.
Delivery of the posterior shoulder.
Place baby skin to skin on maternal chest.
Indications for operative delivery: (1) prolonged or arrested second stage. (2) suspicion of immediate or potential fetal compromise. (3) shortening of the second stage for maternal benefit.
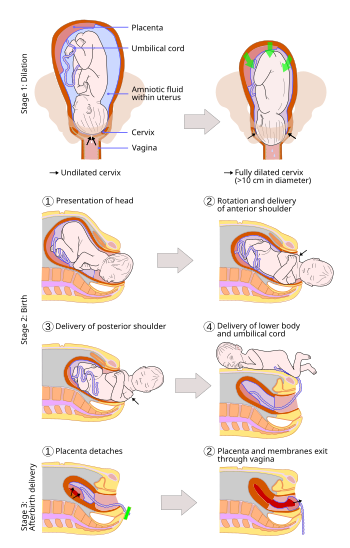
Delivery of the placenta
stage 3 of labor
Active vs expectant management: some sources say active management can help reduce postpartum hemorrhage. Active management includes fundal massage, gentle cord traction, IV/ IM oxytocin.
Placental separation signs: gush of blood, lengthening of the umbilical cord.
Palpate uterus to ensure it is firm and contracted and check to see if all of the placenta was removed by examining the placenta.
Checklist for patient in labor
- establish gestational age: LMP, sonogram, fundal height
- review record for any medical/obstetric/fetal complications & history
- review routine screening tests e.g. GBS
- fetal check:
- external Doppler or bedside ultrasound for fetal viability
- Leopold’s maneuvers/ vaginal exam/ bedside ultrasound to get fetal presentation & estimated fetal weight
- maternal check:
- pelvis exam – adequacy of pelvis
- cervical status and membrane status – cervical dilation & effacement
- prophylaxis if needed eg. antibiotics for GBS
- Monitoring:
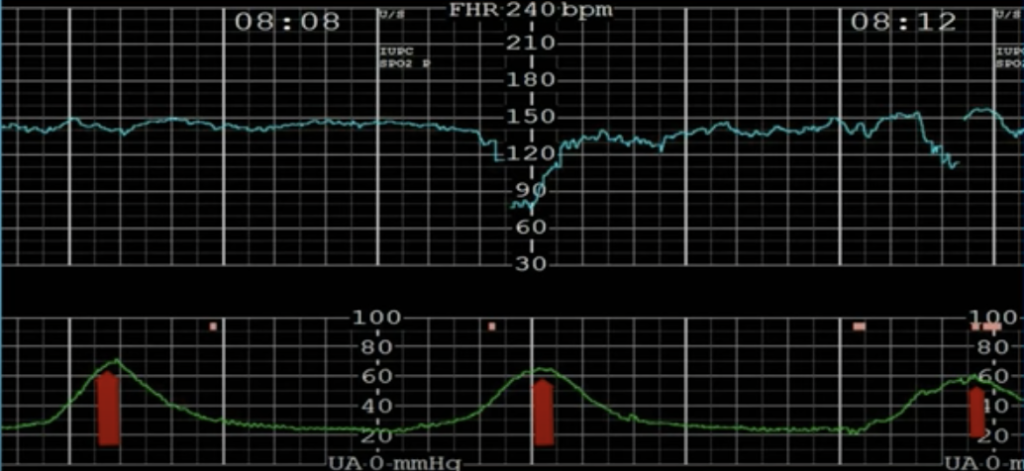
- fetal HR monitor (FHR): external tocometry/ internal and intermittent/continuous
- Uterine contraction monitoring: external/ internal
- Serial checks of labor progression: dilation, effacement, station
- dilation: from 0 cm to 10 cm
- effacement: from 0% to 100%
- station:
- -2 = 2 cm above ischial spine
- -1 = 1 cm above ischial spine
- 0 = at ischial spine
- +1 = 1 cm below it
- +2 = 2 cm below it
- +3 = 3 cm below it
- +4 = 4 cm below it
- +5 = 5 cm below it
- Serial checks of maternal pain
- viceral pain (T10-L1) due to contractions & cervical dilation
- somatic pain (S2-S4 pudendal nerve) due to fetal head pressure on pelvic floor, vagina, and perineum
- can give systemic narcotics, local anesthetics, pudendal block, paracervical block, continuous lumbar epidural (most effective method in the USA), or patient can choose to forgo pain meds or use other methods (eg Lamaze/ breathing techniques)
Abnormal labor
Power, Passenger, Passage
Abnormal Stage 1 of Labor
Power (uterine contractions): ideally 3 times/ 10 minute period.
- Timing of contractions is checked with the external tocometer.

- Strength of contractions is checked with an intrauterine pressure catheter (IUPC). A Montevideo unit (MVU) is the amplitude above the baseline for a 10 minute period and adding it up for the contractions. Ideally >200 MVU is good strength for contractions.
If strength of contractions is inadequate it can be augmented:
- Amniotomy (rupture of amniotic membranes –> prostaglandin release which augments strength of contractions, and allows for fetal head to be the dilating force).
- Oxytocin can strengthen contractions but don’t want them to be too strong = uterine tachysystole (5 contractions/10 minutes for over 30 minutes).
Abnormal Stage 2 of Labor
Passenger (fetus): fetal size i.e. estimated fetal weight >4500 grams increases risk of shoulder/labor dystocia. Fetal position should be occiput anterior position. If occiput posterior or occiput transverse positions lead to bigger diameter which needs to fit through the pelvis increasing risk of dystocia. Same with face presentation.
- Shoulder dystocia: anterior shoulder caught behind pubic symphysis
- McRoberts Maneuver: hyperflexion & abduction of the hips to open up space which can allow the shoulder to be reduced
- Suprapubic pressure: pressure downward on the anterior shoulder

- If these first 2 steps don’t deliver the shoulder, next try to deliver the posterior shoulder and an episoiotmy can help open up space for delivery of the shoulder. Other steps:
- woodscrew/rubin maneuver: rotation of the fetus to reduce the shoulder
- move patients to hands/knees
- intentional clavicular fracture
- Zavenelli procedure: reversing the cardinal movements of labor, putting head back in and performing a cesarean section.
- Cord prolapse: cord comes out before fetus. seen typically when the fetus is not vertex (head first), or when there is spontaneous/ artificial rupture of membranes before the vertex is well engaged.
- put fetal head back up with your hand before it puts more pressure onto the cord
- manually reduce the cord
- hold the fetal head in place (don’t let it descend) until cesarean delivery is completed
Passage (birth canal): cephalopelvic disproportion can be due to the bones of the pelvis or excess fat.
