Acute coronary syndromes
Unstable angina & NSTEMI
same tx for both. MONABASH + PCTA within 24h. Aspirin + clopidogrel = DAPT (dual antiplatelet therapy), and is a key part.
PCTA = PCI. Percutaneous transluminal coronary angioplasty, Percutaneous coronary intervention.
MONABASH
- Monitor
- Oxygen supplementation if SaO2<90%
- Nitroglycerin (sublingual) for pain
- Antiplatelet (aspirin + clopidogrel)
- Beta-blockers (BBs) — reduce oxygen demand in heart
- Anticoagulation e.g. UFH, enoxaparin, fondaparinux
- Statins (High-dose)
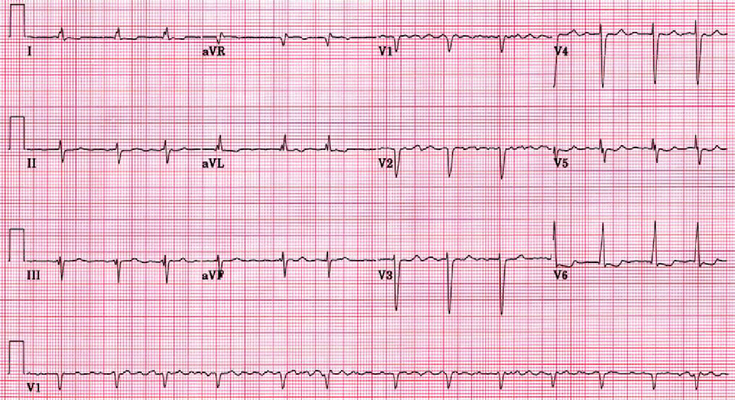
STEMI
- stabilize & MONABASH.
- Reperfusion = PCTA if <90 min, tPA if >120 min eg. IV alteplase. Has to be <12h since symptoms began
- + IV furosemide if severe pulmonary edema
- + IV atropine if unstable sinus bradycardia
- + IV morphine if persistent pain (severe)
- +IV NTG if severe pain/ HTN/ HF
- Avoid these
- BBs if hypotension, bradycardia or heart failure
- IV NTG if hypotension, or RV infarct, or severe aortic stenosis
- Furosemide if hypotension
So, if STEMI with hypotension, MOAASHA –> monitor, O2, antiplatelet, anticoagulation, statin-high-dose, atropine
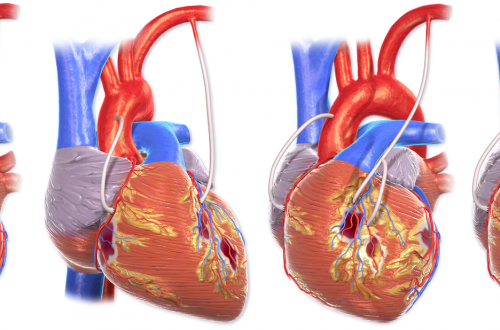
Post-MI Complications
| Complication | Timing | Echocardiogram | ||
|---|---|---|---|---|
| RV failure | RCA occlusion | acute | no blood to lungs –> clear lungs hypotension kussmaul’s sign | hypkinetic RV |
| Papillary muscle rupture | RCA occlusion | 0-5 days later | MR (mitral regurgitation) –> pulmonary edema & new holosytolic murmur at apex | “flail” leaflet of MV |
| Interventricular septum rupture | LAD (apical septum)/ RCA (basal septum) occlusion | 0-5 days later | similar to “VSD” –> holosytolic murmur @LSB “new” more (L–>R shunt) blood to lungs –> pulmonary edema | L–>R shunt ↑O2 from RA to RV |
| Free wall rupture | LAD occlusion | <5 days — 2 wks most (50%) <5 days later (0-5 days) | chest pain, tamponade (shock, distant heart sounds) | pericardial effusion with tamponade |
| LV aneurysm | LAD occlusion | upto several months later (0-months) | subacute heart failure. Stable angina | thin & dyskinetic wall |
Free online practice questions
- Question 1, answer 1 — MKSAP
- Question 2 with answer — Kaplan