-
Aspiration Pneumonia
Caused by anaerobes e.g. Peptostreptococcus, Fusobacterium, Bacteroides, Prevotella Risk factors include an altered level of consciousness which is often due to: seizures, brain injury, dementia generalized anesthesia or sedation drug or alcohol intoxication elderly Aspiration most often occurs on the right side because the right main stem bronchus is larger and more vertical than the left Symptoms can include cough, fever, dyspnea on exertion Aspiration pneumonia often leads to lung abscesses
-
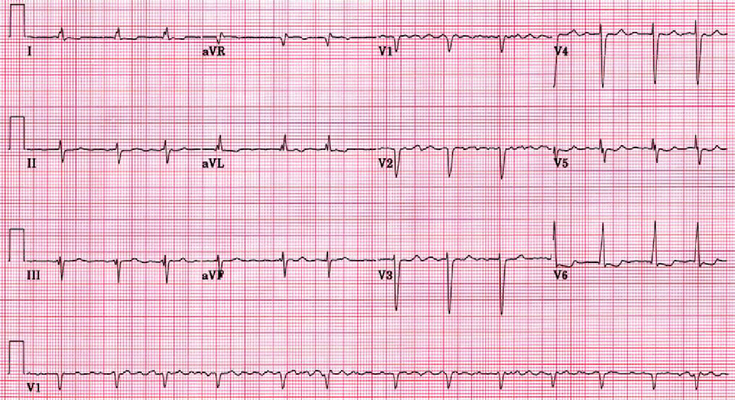
Atrial Fibrillation (Afib)
Acute atrial fibrillation with rapid ventricular rate If patient is experiencing symptoms get an IV placed and cardiac monitoring started If the patient is hemodynamically unstable give them synchronized cardioversion with rapid ventricular rate the goal is to get the heart rate below 110 bpm, and this is done with rate control medications. Find out if they have heart failure (acute decompensated heart failure) – if yes, then they will usually get digoxin or amiodarone. If no, then a calcium channel blocker like diltiazem or a beta-blocker like metoprolol If they received electrical cardioversion they will need anticoagulation for 1 month Chronic Atrial fibrillation Rate and Rhythm control have similar…
-
Pneumonia
Outpatient Are there risk factors for MRSA or pseudomonas (e.g. had MRSA or pseudomonas previously or was recently hospitalized and received IV antibiotics in the last 90 days)? Are there comorbidities e.g. chronic heart, lung, liver or kidney disease, diabetes mellitus, alcoholism or asplenia? No: Amoxicillin 1 g tid OR Doxycycline 100 mg bid OR a macrolide if local pneumococcal resistance is < 25%. Macrolide options include: Azithromycin 500 mg on day 1 then 250 mg daily OR Clarithromycin ER 1g daily OR Clarithromycin 500 mg bid. Note that the strongest recommendation is for amoxicillin, followed by a conditional recommendation for doxycycline (there is limited data for oral doxycycline use…
-
Stroke and TIA
Stroke symptoms last ≥24 hours Stroke results in permanent neurologic deficits Stroke can be due to hemorrhage (20%) or ischemia (80%) Stroke with no known cause is called cryptogenic Stroke spares the upper 1/3 of the face TIA symptoms last <24 hours TIA symptoms resolve completely TIA can only be due to ischemia (emboli or thrombus) – because hemorrhage would take >24 hours to resolve TIA does not spare the upper 1/3 of the face Artery localization The artery affected in stroke or TIA can be localized based on the symptoms. Anterior Cerebral Artery (ACA) Mainly lower extremity weakness Urinary incontinence Personality changes or psychiatric symptoms Middle Cerebral Artery (MCA)…
-
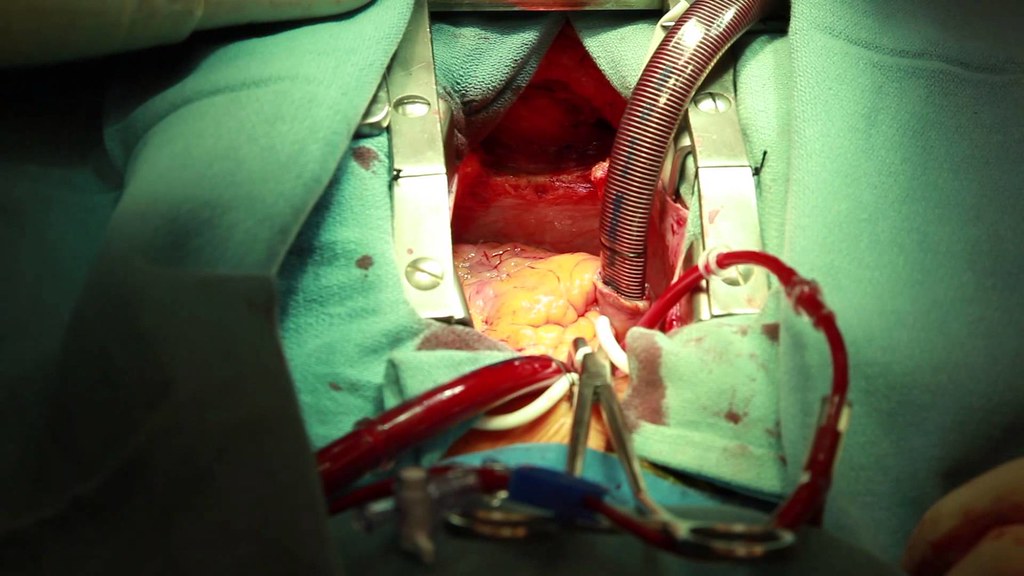
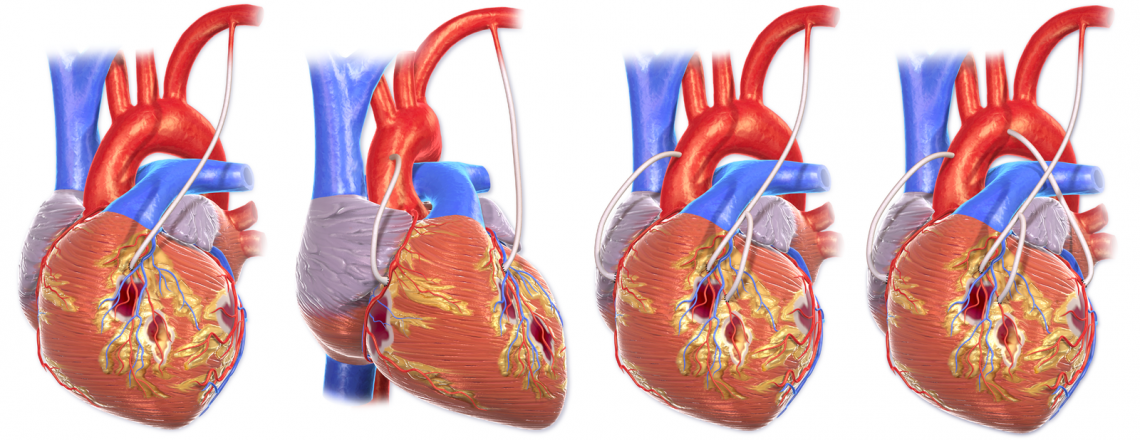
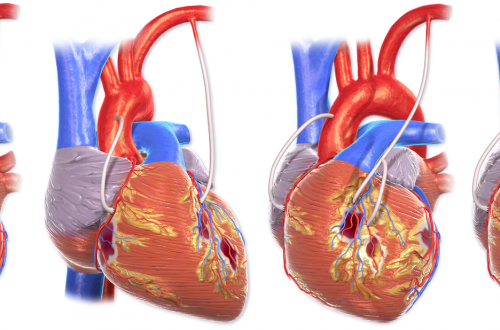
Coronary Artery Bypass Grafting
The goal of CABG is to restore blood flow to the myocardium. Preoperative Care During preoperative assessment of patients undergoing coronary artery bypass grafting, special care should be paid to the severity of their coronary artery disease, their vascular function, the presence of comorbid disease, and explaining to the patient the procedure and postoperative care expectations. Medications Cardiac medications are to be continued up to the morning of the operation, except ACE inhibitors and digoxin. Monitoring Routine monitoring of CABG patients often includes: 5 lead ECG Temperature – core temperature (nasopharyngeal) Pulse oxymetry Capnography Central venous pressure Invasive BP monitoring Anesthesia for CABG An example protocol for induction: Etomidate, Fentanyl,…
-
Chest Pain
Intravenous Fluid Orders Intravenous Cannula – Insert IV Peripheral Saline Flush/Lock: Saline Lock IV Maintenance: 0.9% NaCl infusion at ______ mL/hour, reassess after hours lactated ringers infusion at ______ mL/hour, reassess after hours IV Bolus: 0.9% NaCl ______ mL over ______ hour(s) lactated ringers _______ mL over _______ hour(s) Laboratory Investigations Hematology Complete Blood Count (CBC) PT INR Chemistry Troponin Repeat Troponin_________time(s) (specify collection time below) ___________:_____________ ___________:_____________ Electrolytes (Na, K, Cl, CO2) Glucose Creatinine Urea Serum bHCG Urine Tests Urine Dipstick Testing – POCT Urinalysis Pregnancy Test, Urine (POCT if available) Other Labs (based on presentation needs of the patient) Diagnostic Imaging Chest x-ray usually indicated unless recently performed to rule out…
-
Acute Coronary Syndromes
Checklist ECG: Get a 12 lead ECG within 10 minutes of patient presenting with chest pain Vitals: Take initial vital signs: temp, HR, RR, SpO2, BP in both arms; and repeat if there further chest pain or equivalent symptoms Oxygen: Give Oxygen if SpO2 ≤ 90% or there are clinical signs of hypoxemia Antiplatelets: Give acetylsalicylic acid (Aspirin®) now if it was not given prior to arrival at hospital. Write down when it was given. Nitroglycerin: Give Nitroglycerin in hemodynamically stable patients every 5 minutes as needed. *Avoid if suspected RV infarction. Dose: usually 0.3 to 0.4 mg. Place defibrillation pads on chest – because there is a high risk…
-
Endocrinology – topics
Hypothalamus & Pituitary Neuroendocrinology Pituitary masses and tumors Posterior pituitary disorders Thyroid Diagnostic testing for suspected thyroid disease Hyperthyroidism Hypothyroidism & Thyroiditis Nontoxic diffuse goiter Thyroid nodule Thyroid cancer Adrenal Cortex Adrenal cortex Endocrine hypertension Endocrine pancreas Type 2 diabetes mellitus Type 1 diabetes mellitus Hypoglycemia Obesity Lipid disorders Mineral Metabolism Osteoporosis Rickets & Osteomalacia Kidney stones Reproductive endocrinology Hormonal contraception Hormonal therapies Testicular disorders Pregnancy and endocrine changes Pediatric endocrinology Disorders of sexual development Growth disorders Multi-organ endocrine disorders Multiple endocrine metaplasia (MEN) HIV/AIDs – endocrine problems
-
Sarcoidosis
multisystem disease characterized by non-caseating granulomas etiology is unknown Presentation Lungs: dry, non-productive cough, dyspnea, chest pain Eyes: blurry vision, conjunctivitis, eye pain, uveitis (common), iritis Skin: erythema nodosum, papules, macules, nodules, lupus pernio Heart: arrhythmias, cardiomyopathy Diagnosis diagnosis of exclusion initial labs: CBC, serum chemistry (ALT, AST, ALP, BUN, Cr, Ca, other electrolytes), urinalysis, 24 h urine excretion of calcium, CRP, ESR, tuberculin skin test imaging: CXR, ECG pulmonary function tests: spirometry, diffusion capacity of carbon monoxide (DLCO)- single breath biopsy (skin, lymph nodes or conjunctiva) of affected area, and if no suitable area is present then bronchoscopy with transbronchial biopsy. Management Corticosteroids are the mainstay therapy when required.…
-
Hypercalcemia
Normal Ca in mg/dL: 8.4 – 10.2 (lab value from nbme.org) Normal Ca in mmol/L: 2.18 – 2.58 (lab value from mcc.ca) Sample Case: A 40 year old man arrives in the clinic complaining of polyuria, constipation and malaise. He has normal vital signs and no significant findings on physical exam. On laboratory testing, his serum calcium is elevated at 11 mg/dL (2.74 mmol/L). What is the best next step in management? First, you need to recognize that he has hypercalcemia. The most common cause of hypercalcemia in patients arriving in the clinic is primary hyperparathyroidism. To diagnose hyperparathyroidism, you first need to get the parathyroid hormone (PTH) level. Remember,…