-
Manometry
Esophageal manometry is an accurate method for assessing esophageal motility disorders including achalasia, diffuse esophageal spasm and scleroderma affecting the esophagus.
-
Dysphagia Qs
Loading…
-
Esophagus in Scleroderma
IM→GI→Esophagus→Motility Disorders→Scleroderma A 35 year old African American woman presents to your clinic with difficulty swallowing and heart burn. History reveals a diagnosis of scleroderma. Pathology: Scleroderma causes diffuse fibrosis of the esophagus which results in loss of LES (lower esophageal sphincter) function as well as absent peristalsis of smooth muscle in the distal esophagus. Presentation: Patients present with dysphagia as well as GERD. They will have history of scleroderma, look for a description of Raynaud’s phenomenon. Diagnosis: Manometry will show hypotensive/ absent peristalsis and LES tone. Management: Proton pump inhibitors (PPIs).
-
Diffuse esophageal spasm (DES)
A 32 year old comes to your clinic complaining of difficulty swallowing with solids, as well as both hot and cold liquids. This has been happening intermittently for about a week. Pathology Impaired innervation of the esophagus –> uncoordinated simultaneous contractions (non-peristaltic). This primarily affects the distal esophagus, so this condition is also called Distal Esophageal Spasm (DES). Presentation Spontaneous odynophagia and dysphagia with both solids and liquids. May be described as “chest pain” when eating. Often precipitated by emotional stress. The chest pain is relieved by nitroglycerin and calcium channel blockers — they relax the esophageal myocytes. They often have regurgitation of food. Key features: – progressive dysphagia to…
-
Bronchiolitis
Preview Questions What is the recommended management of bronchiolitis according to the American Academy of Pediatrics? What is the most common pathogen responsible for bronchiolitis? What happens to the airways in bronchiolitis? Which patients require admission to hospital? When is Palivizumab considered? About Bronchiolitis Bronchiolitis is the most common reason for infants to be hospitalized during the first year of life Bronchiolitis is most often seen in infants 3 to 6 months old Bronchiolitis Pathogens causing Bronchiolitis Bronchiolitis is most often due to viral infection of the lower respiratory tract. The most common virus responsible for bronchiolitis is respiratory syncytial virus (RSV). Other viruses that can cause bronchiolitis include human…
-
Aspiration Pneumonia
Caused by anaerobes e.g. Peptostreptococcus, Fusobacterium, Bacteroides, Prevotella Risk factors include an altered level of consciousness which is often due to: seizures, brain injury, dementia generalized anesthesia or sedation drug or alcohol intoxication elderly Aspiration most often occurs on the right side because the right main stem bronchus is larger and more vertical than the left Symptoms can include cough, fever, dyspnea on exertion Aspiration pneumonia often leads to lung abscesses
-
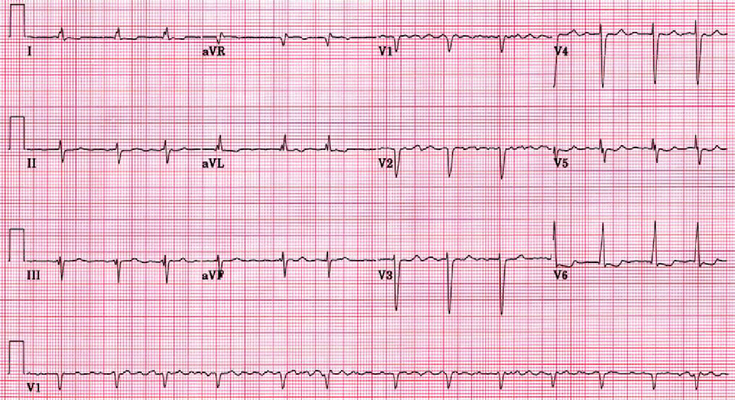
Atrial Fibrillation (Afib)
Acute atrial fibrillation with rapid ventricular rate If patient is experiencing symptoms get an IV placed and cardiac monitoring started If the patient is hemodynamically unstable give them synchronized cardioversion with rapid ventricular rate the goal is to get the heart rate below 110 bpm, and this is done with rate control medications. Find out if they have heart failure (acute decompensated heart failure) – if yes, then they will usually get digoxin or amiodarone. If no, then a calcium channel blocker like diltiazem or a beta-blocker like metoprolol If they received electrical cardioversion they will need anticoagulation for 1 month Chronic Atrial fibrillation Rate and Rhythm control have similar…
-
Pneumonia
Outpatient Are there risk factors for MRSA or pseudomonas (e.g. had MRSA or pseudomonas previously or was recently hospitalized and received IV antibiotics in the last 90 days)? Are there comorbidities e.g. chronic heart, lung, liver or kidney disease, diabetes mellitus, alcoholism or asplenia? No: Amoxicillin 1 g tid OR Doxycycline 100 mg bid OR a macrolide if local pneumococcal resistance is < 25%. Macrolide options include: Azithromycin 500 mg on day 1 then 250 mg daily OR Clarithromycin ER 1g daily OR Clarithromycin 500 mg bid. Note that the strongest recommendation is for amoxicillin, followed by a conditional recommendation for doxycycline (there is limited data for oral doxycycline use…
-
Stroke and TIA
Stroke symptoms last ≥24 hours Stroke results in permanent neurologic deficits Stroke can be due to hemorrhage (20%) or ischemia (80%) Stroke with no known cause is called cryptogenic Stroke spares the upper 1/3 of the face TIA symptoms last <24 hours TIA symptoms resolve completely TIA can only be due to ischemia (emboli or thrombus) – because hemorrhage would take >24 hours to resolve TIA does not spare the upper 1/3 of the face Artery localization The artery affected in stroke or TIA can be localized based on the symptoms. Anterior Cerebral Artery (ACA) Mainly lower extremity weakness Urinary incontinence Personality changes or psychiatric symptoms Middle Cerebral Artery (MCA)…
-
Approach to Chest Pain
Chest pain is one of the most common presenting complaints. There are many causes of chest pain ranging from cardiac to gastrointestinal problems. However, there are a few critical or life-threatening diagnoses causing chest pain that must not be forgotten. Can you list at least 6 potentially life-threatening causes of chest pain? Acute coronary syndrome (ACS) Aortic dissection Pulmonary embolism (PE) Pneumothorax Pericarditis with tamponade Esophageal rupture Why does the pain in chest pain radiate to other locations such as the arms? “Referred Pain” Somatic afferent fibers synapse on the same dorsla root ganglia as the thoracic viscera, and chest pain can be mistakenly perceived as originating from the arms,…